Clostridium species, notably Clostridium perfringens, are anaerobic, gram-positive bacteria commonly residing in the human gastrointestinal tract. While typically harmless, these organisms can become pathogenic under certain conditions, leading to severe infections, including pelvic cellulitis. This article delves into the etiology, clinical manifestations, diagnostic methodologies, and treatment protocols associated with clostridial pelvic cellulitis.
Etiology and Pathogenesis
Clostridial pelvic infections often arise from disruptions in mucosal barriers, allowing the translocation of bacteria from the gastrointestinal or female genital tract into sterile pelvic tissues. Factors contributing to such disruptions include:
- Surgical Procedures: Pelvic surgeries can inadvertently introduce clostridial bacteria into deeper tissues.
- Trauma: Injuries compromising the integrity of pelvic structures may facilitate bacterial invasion.
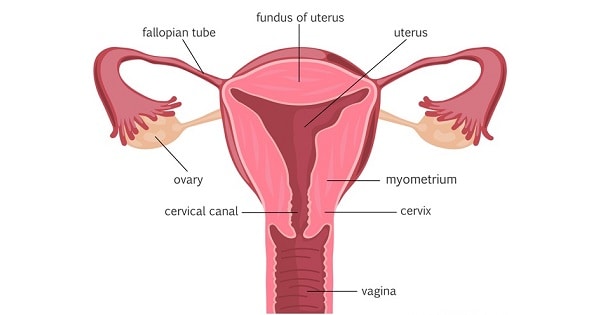
- Gynecological Conditions: Procedures like childbirth or septic abortions have been associated with clostridial uterine infections.
Once introduced, C. perfringens produces potent exotoxins, such as alpha-toxin (lecithinase), which disrupt cell membranes, leading to tissue necrosis and gas formation. This necrotizing process can rapidly progress, resulting in systemic toxicity.
Clinical Manifestations
The presentation of clostridial pelvic cellulitis can vary but commonly includes:
- Abdominal Pain: Patients often report severe, localized pain in the lower abdomen.
- Fever: Elevated body temperature is a frequent finding.
- Vaginal Discharge: A foul-smelling, bloody discharge may be evident, particularly in uterine involvement.
- Gas Formation: Crepitus or palpable gas in the pelvic region can be detected due to bacterial gas production.
In advanced cases, systemic manifestations such as hypotension, tachycardia, jaundice, and oliguria may indicate the development of clostridial sepsis, a life-threatening condition.
Diagnostic Approaches
Prompt diagnosis is crucial for effective management. Recommended diagnostic steps include:
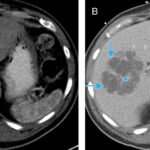
- Imaging Studies: X-rays or CT scans can reveal gas accumulation in pelvic tissues, a hallmark of clostridial infection.
- Microbiological Analysis: Gram staining and culture of samples from the infection site, pus, or blood can identify gram-positive rods characteristic of Clostridium species.
- Laboratory Tests: Elevated white blood cell counts, hemolysis, and renal function abnormalities may be observed.
Early and repeated sampling enhances diagnostic accuracy, facilitating timely intervention.
Treatment Strategies
Management of clostridial pelvic cellulitis necessitates a multifaceted approach:
- Surgical Intervention: Immediate debridement of necrotic tissue is essential to halt disease progression. In severe cases, organ removal, such as hysterectomy, may be lifesaving.
- Antibiotic Therapy: High-dose intravenous penicillin G is the standard treatment. Alternatives include carbapenems, beta-lactam/beta-lactamase inhibitors, metronidazole, or clindamycin. Combining clindamycin with penicillin is beneficial due to its ability to suppress toxin production.
- Supportive Care: Management of sepsis, including fluid resuscitation, vasopressor support, and renal replacement therapy in cases of acute renal failure, is critical.
Early recognition and aggressive treatment are pivotal in improving patient outcomes.