Clostridium Liver Abscess, notably Clostridium perfringens and Clostridium septicum, are anaerobic, gram-positive bacilli implicated in various human infections. Among these, liver abscesses, though uncommon, represent severe clinical entities necessitating prompt recognition and intervention.
Etiology and Pathogenesis
Clostridium liver abscesses typically arise from:
- Hematogenous Spread: Bacteria translocate from the gastrointestinal tract or other primary sites via the portal vein.
- Direct Extension: Infection spreads from adjacent structures, such as the biliary tree.
- Trauma: Blunt abdominal injuries can predispose the liver to abscess formation.
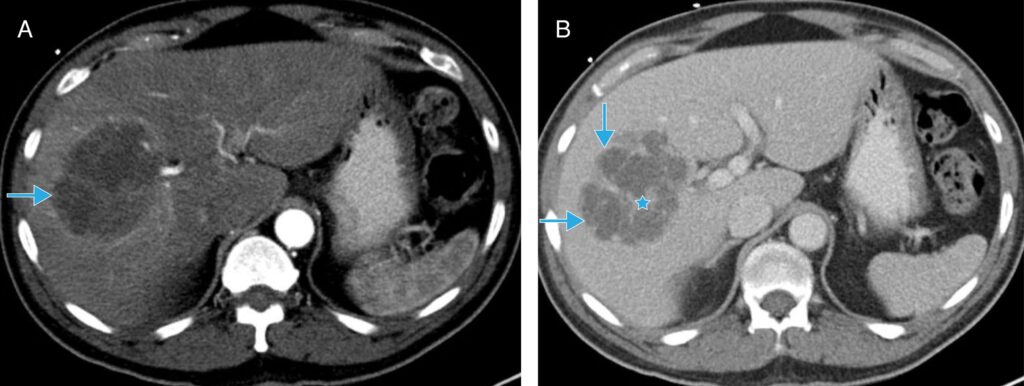
Notably, C. perfringens is renowned for its rapid replication and potent exotoxin production, leading to gas formation within tissues. This gas production is a hallmark of clostridial infections and can be visualized radiologically.
Clinical Manifestations
Patients with clostridial liver abscesses may present with:
- Fever and Chills: Indicative of systemic infection.
- Right Upper Quadrant Pain: Localized hepatic discomfort.
- Jaundice: Resulting from biliary involvement or hemolysis.
- Hemolytic Anemia: Particularly associated with C. perfringens, due to its hemolysin production.
The rapid progression of symptoms is characteristic, often leading to septic shock if not promptly addressed.
Diagnostic Approaches
Accurate diagnosis involves:
- Imaging Studies:
- Ultrasonography: Initial modality to detect abscesses.
- Computed Tomography (CT): Superior in identifying gas-forming abscesses, a distinctive feature of clostridial infections.
- Microbiological Analysis:
- Blood Cultures: May reveal clostridial bacteremia.
- Aspiration and Culture of Abscess Contents: Confirms the causative organism.
Early identification is crucial due to the fulminant nature of clostridial infections.
Treatment Strategies
Management encompasses:
- Antibiotic Therapy:
- Empirical Coverage: Initiate broad-spectrum antibiotics targeting anaerobes.
- Targeted Therapy: Adjust based on culture sensitivities, commonly involving penicillin or metronidazole.
- Surgical Intervention:
- Percutaneous Drainage: Preferred for accessible abscesses.
- Open Surgical Drainage: Reserved for cases unresponsive to percutaneous methods or with multiple loculations.
Given the aggressive progression, a combination of prompt surgical drainage and appropriate antibiotics is imperative.
Prognosis
Despite advancements in medical care, clostridial liver abscesses are associated with high morbidity and mortality rates. Early detection and aggressive treatment are pivotal in improving outcomes.