Urinary tract infections (UTIs) represent a significant portion of nosocomial infections, accounting for approximately 40% of hospital-acquired cases. Among the diverse pathogens responsible, the genus Citrobacter has emerged as a notable contributor. This article delves into the intricacies of Citrobacter-induced UTIs, encompassing their etiology, clinical manifestations, diagnostic procedures, therapeutic approaches, and preventive measures.
Etiology of Citrobacter UTIs
Citrobacter species are aerobic, Gram-negative bacilli belonging to the Enterobacteriaceae family. Ubiquitously present in water, soil, food, and the intestines of humans and animals, these bacteria are opportunistic pathogens. Notably, Citrobacter accounts for 5% to 12% of bacterial isolates in adult UTIs. The two primary species implicated are:
- Citrobacter koseri: Predominantly associated with UTIs, accounting for 72.4% of cases in certain studies.
- Citrobacter freundii: Less frequently isolated but still clinically significant.
Risk Factors
Several factors predispose individuals to Citrobacter UTIs:
- Hospitalization: Increased exposure to nosocomial pathogens.
- Indwelling Urethral Catheterization: Facilitates bacterial entry into the urinary tract.
- Genitourinary Instrumentation: Procedures that may introduce bacteria.
- Obstructive Uropathy: Conditions like prostatic enlargement leading to urinary stasis.
- Elderly Age: Particularly males, due to factors such as prostatic hypertrophy and decreased bactericidal activity of prostatic secretions.
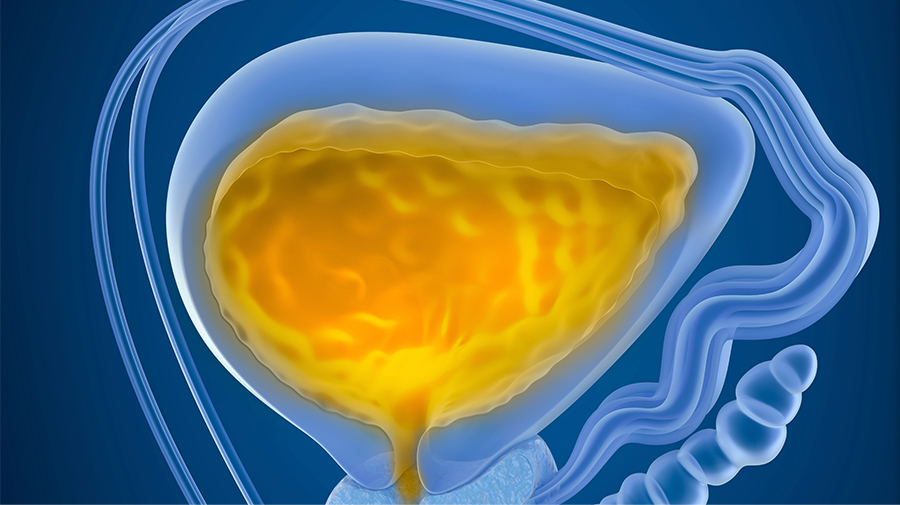
Clinical Manifestations
The symptoms of Citrobacter UTIs are akin to those caused by other uropathogens and may include:
- Dysuria (painful urination)
- Increased urinary frequency and urgency
- Hematuria (blood in urine)
- Lower abdominal or suprapubic pain
- Fever and chills in cases of upper tract involvement
Diagnostic Procedures
Accurate diagnosis is pivotal for effective management. The following steps are recommended:
- Urine Culture: Isolation and identification of Citrobacter species using standard microbiological techniques.
- Antibiotic Susceptibility Testing: Conducted via the disc diffusion method on Mueller-Hinton agar, adhering to Clinical and Laboratory Standards Institute (CLSI) guidelines.
Antimicrobial Resistance Patterns
A concerning aspect of Citrobacter UTIs is their notable resistance to multiple antibiotics. Studies have highlighted:
- High resistance rates to amoxicillin and ampicillin, rendering them ineffective.
- Increasing resistance to trimethoprim and amoxiclav over the past decade.
- Significant resistance to cefotaxime, cephalexin, norfloxacin, ciprofloxacin, and aminoglycosides.
Given these patterns, nitrofurantoin has demonstrated good in vitro activity and may be considered a first-line oral therapy for ambulatory patients.
Treatment Strategies
Management of Citrobacter UTIs should be guided by susceptibility profiles:
- Empirical Therapy: Initiate with agents like nitrofurantoin, especially in outpatient settings.
- Definitive Therapy: Tailor based on culture and sensitivity results, considering the high rates of resistance to commonly used antibiotics.
Prevention Measures
Preventing Citrobacter UTIs involves:
- Judicious use of urinary catheters and minimizing their duration.
- Adherence to aseptic techniques during genitourinary instrumentation.
- Regular monitoring of antimicrobial susceptibility patterns to inform empirical therapy.
- Prudent use of antibiotics to mitigate the emergence of resistance.

