Acute exacerbation of obstructive chronic bronchitis (AECB) is a critical condition that worsens chronic obstructive pulmonary disease (COPD). Among the bacterial pathogens responsible, Haemophilus influenzae (H. flu) is one of the most common culprits. This Gram-negative coccobacillus contributes significantly to COPD exacerbations, leading to increased morbidity and healthcare burden. Understanding its pathophysiology, risk factors, clinical presentation, and management is essential for optimal patient care.
Pathophysiology of H. flu-Induced AECB
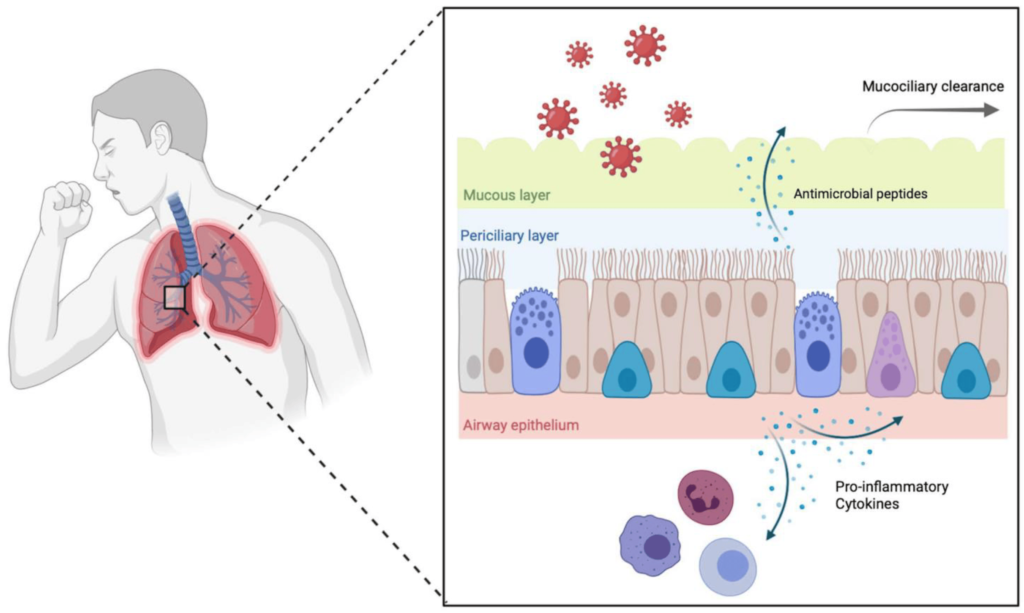
H. flu colonizes the lower respiratory tract, triggering an inflammatory cascade that leads to increased mucus production, bronchial obstruction, and impaired gas exchange. The pathogen’s ability to evade host immunity exacerbates airway inflammation and lung function decline.
Several factors increase susceptibility to H. flu-induced AECB, including:
- Smoking: Damages airway defenses, facilitating bacterial colonization.
- Advanced Age: Weakened immune response enhances infection risk.
- Chronic Lung Disease: COPD and bronchiectasis increase vulnerability.
- Environmental Exposure: Pollutants and allergens exacerbate respiratory inflammation.
- Immunosuppression: Conditions such as diabetes and corticosteroid use increase risk.
Clinical Symptoms
Patients experiencing AECB due to H. flu commonly present with:
- Increased Sputum Production: Thick, purulent sputum with a yellow-green color.
- Worsening Dyspnea: Progressive shortness of breath.
- Persistent Cough: Often productive with increased mucus.
- Fever and Malaise: Systemic signs indicating bacterial infection.
- Wheezing and Chest Tightness: Due to airway inflammation and mucus buildup.
Diagnosis
Diagnosis involves:
- Clinical Examination: Assessing symptom severity and history of COPD.
- Sputum Culture and Gram Staining: Identifies H. flu as the causative agent.
- Pulmonary Function Tests (PFTs): Evaluates lung function deterioration.
- Chest X-ray or CT Scan: Detects lung inflammation and infection.
- C-reactive Protein (CRP) and Procalcitonin Levels: Helps differentiate bacterial from viral exacerbations.
Treatment Strategies
1. Antibiotic Therapy
- First-line antibiotics: Amoxicillin-clavulanate, fluoroquinolones (levofloxacin, moxifloxacin), and macrolides (azithromycin, clarithromycin).
- Beta-lactamase inhibitors: Combat resistance seen in some H. flu strains.
- Alternative options: Second-generation cephalosporins or doxycycline for resistant cases.
2. Bronchodilators and Corticosteroids
- Short-acting beta-agonists (SABAs): Albuterol for immediate relief.
- Long-acting bronchodilators (LABAs): Formoterol and salmeterol for sustained control.
- Inhaled corticosteroids (ICS): Budesonide or fluticasone to reduce inflammation.
3. Oxygen Therapy
- Supplemental oxygen: For patients with hypoxemia.
- Non-invasive ventilation (NIV): Used in severe respiratory distress.
4. Pulmonary Rehabilitation
- Breathing exercises: Enhances lung function and capacity.
- Nutritional support: Maintains overall health and immune response.
- Physical activity: Strengthens respiratory endurance.
Prevention Strategies
- Smoking Cessation: Significantly reduces exacerbation risk.
- Vaccination: Annual influenza and pneumococcal vaccines protect against respiratory infections.
- Hand Hygiene and Respiratory Protection: Minimizes bacterial transmission.
- Regular Pulmonary Check-ups: Ensures early detection and management of symptoms.
Prognosis and Complications
Patients with recurrent AECB due to H. flu are at increased risk for:
- Chronic Respiratory Failure
- Frequent Hospitalizations
- Higher Mortality Rates
- Secondary Infections
Timely diagnosis and effective treatment improve patient outcomes and reduce the long-term burden of COPD exacerbations.
Acute exacerbation of obstructive chronic bronchitis due to H. flu is a severe respiratory condition requiring prompt medical intervention. A combination of antibiotic therapy, bronchodilators, corticosteroids, and preventive measures is crucial for managing this condition effectively. Increased awareness and improved treatment protocols can enhance patient quality of life and reduce disease burden.