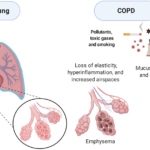
Acute Exacerbation of Obstructive Chronic Bronchitis by Streptococcus pneumoniae is a significant cause of morbidity in patients with chronic obstructive pulmonary disease (COPD). Among bacterial pathogens, Streptococcus pneumoniae (S. pneumoniae) is a leading cause of exacerbations, leading to increased airway inflammation, excessive mucus production, and impaired lung function. Understanding the pathophysiology, risk factors, symptoms, and management of S. pneumoniae-induced AECB is crucial for improved patient outcomes.
Pathophysiology of S. pneumoniae-Induced AECB
S. pneumoniae is a Gram-positive, encapsulated bacterium that colonizes the upper respiratory tract and can descend into the bronchi, leading to severe inflammation. The bacteria evade immune responses through their polysaccharide capsule, triggering cytokine release and neutrophilic infiltration, worsening airflow obstruction and exacerbation symptoms.

Risk Factors
Factors that predispose individuals to S. pneumoniae-induced AECB include:
- Smoking: Impairs mucociliary clearance and immune defense.
- Advanced Age: Reduces immune response effectiveness.
- COPD and Chronic Lung Disease: Increases airway susceptibility to infection.
- Air Pollution Exposure: Aggravates lung inflammation.
- Comorbidities: Conditions like diabetes and heart disease elevate risk.
Clinical Symptoms
Patients experiencing an exacerbation due to S. pneumoniae often exhibit:
- Increased Sputum Production: Thick, purulent mucus with potential blood streaks.
- Severe Dyspnea: Difficulty breathing, especially with exertion.
- Persistent Cough: Worsening and productive in nature.
- Fever and Chills: Indicative of active bacterial infection.
- Wheezing and Chest Tightness: Caused by airway obstruction.
Diagnosis Acute Exacerbation of Obstructive Chronic Bronchitis by Streptococcus pneumoniae
Accurate diagnosis involves:
- Clinical Evaluation: Assessing COPD history and symptom severity.
- Sputum Culture and Gram Staining: Identifies S. pneumoniae infection.
- Pulmonary Function Tests (PFTs): Measures airflow limitation.
- Chest X-ray or CT Scan: Detects pneumonia or other complications.
- Blood Biomarkers (CRP, Procalcitonin): Differentiates bacterial from viral infections.
Treatment Strategies
1. Antibiotic Therapy
- First-line antibiotics: Amoxicillin-clavulanate, macrolides (azithromycin, clarithromycin), and fluoroquinolones.
- Penicillin-based therapies: Address susceptibility profiles of S. pneumoniae.
- Alternative options: Cephalosporins or tetracyclines for resistant strains.
2. Bronchodilators and Corticosteroids
- Short-acting beta-agonists (SABAs): Albuterol for immediate relief.
- Long-acting bronchodilators (LABAs): Salmeterol and formoterol for sustained airway relaxation.
- Inhaled corticosteroids (ICS): Budesonide or fluticasone to reduce inflammation.
3. Oxygen Therapy
- Supplemental oxygen: For hypoxemic patients.
- Non-invasive ventilation (NIV): Used in severe exacerbations to prevent intubation.
4. Pulmonary Rehabilitation
- Breathing exercises: Strengthens respiratory muscles.
- Nutritional optimization: Supports immune function and recovery.
- Physical therapy: Enhances lung efficiency.
Prevention Strategies
- Smoking Cessation: Reduces exacerbation frequency.
- Vaccination: Annual pneumococcal and influenza vaccines recommended.
- Infection Control Measures: Regular handwashing and respiratory hygiene.
- Routine Health Monitoring: Ensures early detection and intervention.
Prognosis and Complications
Repeated exacerbations due to S. pneumoniae increase the risk of:
- Chronic Respiratory Failure
- Frequent Hospitalizations
- Higher Mortality Rates
- Secondary Pulmonary Infections
Timely diagnosis and tailored treatment approaches significantly improve patient outcomes.
Acute exacerbation of obstructive chronic bronchitis caused by Streptococcus pneumoniae requires prompt medical attention and strategic management. A combination of antibiotic therapy, bronchodilators, corticosteroids, and preventive care plays a vital role in reducing disease burden and improving patient quality of life.