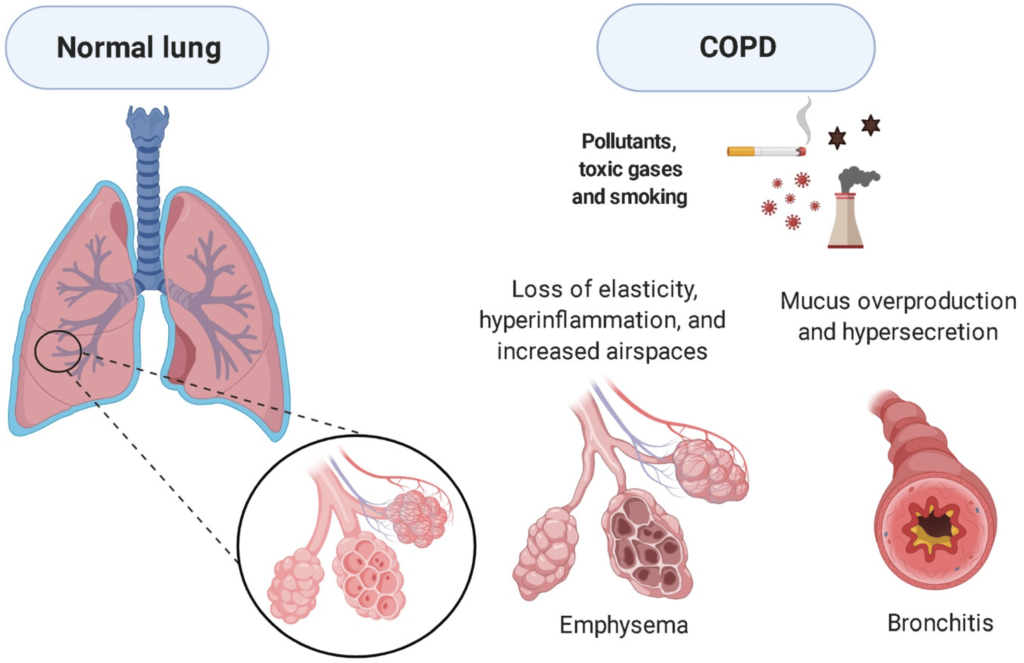
Acute exacerbation of obstructive chronic bronchitis (AECB) is a serious complication of chronic obstructive pulmonary disease (COPD). Among the bacterial pathogens responsible for AECB, Moraxella catarrhalis (M. catarrhalis) plays a crucial role. This Gram-negative diplococcus is known for its increasing antibiotic resistance, making treatment more challenging. Understanding its pathophysiology, risk factors, symptoms, and management is essential for better patient outcomes.
Pathophysiology of M. catarrhalis-Induced AECB
M. catarrhalis colonizes the respiratory tract and exacerbates bronchial inflammation, leading to increased mucus production, airway obstruction, and impaired lung function. The bacterium produces beta-lactamases, contributing to resistance against common antibiotics.
Risk Factors
Several factors increase susceptibility to M. catarrhalis-induced AECB, including:
- Smoking: Damages ciliary function and weakens mucosal defenses.
- Advanced Age: Reduced immune response increases vulnerability.
- Pre-existing COPD: Impaired lung function facilitates bacterial growth.
- Environmental Pollutants: Exposure to pollutants weakens respiratory defenses.
- Comorbidities: Conditions such as diabetes and heart disease increase risk.
Clinical Symptoms
Patients with M. catarrhalis-induced AECB typically present with:
- Increased Sputum Production: Thick, purulent sputum with a yellow-green color.
- Worsening Dyspnea: Shortness of breath, particularly at rest.
- Cough: Persistent and productive cough.
- Fever and Malaise: Systemic symptoms indicating bacterial infection.
- Wheezing and Chest Tightness: Due to airway inflammation and obstruction.
Diagnosis
Diagnosis involves:
- Clinical Assessment: Evaluating symptom severity and history of COPD.
- Sputum Culture and Gram Staining: Confirms M. catarrhalis infection.
- Pulmonary Function Tests (PFTs): Assesses airflow limitation.
- Chest X-ray or CT Scan: Identifies infection-related complications.
- C-reactive Protein (CRP) and Procalcitonin Tests: Differentiates bacterial from viral exacerbations.
Treatment Strategies
1. Antibiotic Therapy
- First-line antibiotics: Amoxicillin-clavulanate, macrolides (azithromycin, clarithromycin), and fluoroquinolones.
- Beta-lactamase inhibitors: Address antibiotic resistance.
- Alternative therapies: Tetracyclines or cephalosporins in resistant cases.
2. Bronchodilators and Corticosteroids
- Short-acting beta-agonists (SABAs): Albuterol for immediate relief.
- Long-acting bronchodilators (LABAs): Formoterol and salmeterol for sustained control.
- Inhaled corticosteroids (ICS): Fluticasone or budesonide to reduce inflammation.
3. Oxygen Therapy
- Supplemental oxygen: For patients with hypoxemia.
- Non-invasive ventilation (NIV): Helps in severe respiratory distress.
4. Pulmonary Rehabilitation
- Breathing exercises: Improves lung capacity.
- Nutritional support: Helps maintain optimal body weight.
- Physical activity: Enhances overall respiratory endurance.
Prevention Strategies
- Smoking Cessation: Reduces the risk of exacerbations.
- Vaccination: Annual influenza and pneumococcal vaccines.
- Hand Hygiene and Respiratory Protection: Prevents bacterial transmission.
- Regular Medical Check-ups: Enables early detection and management of symptoms.
Prognosis and Complications
Patients with recurrent AECB face an increased risk of:
- Chronic Respiratory Failure
- Frequent Hospitalizations
- Increased Mortality Rate
- Secondary Infections
Early diagnosis and appropriate treatment significantly improve outcomes.
M. catarrhalis-induced acute exacerbation of obstructive chronic bronchitis is a severe respiratory condition requiring timely intervention. Effective management involves antibiotics, bronchodilators, corticosteroids, and preventive measures. Raising awareness and improving treatment strategies can enhance patient quality of life and reduce disease burden.