Understanding Chronic Thromboembolic Pulmonary Hypertension
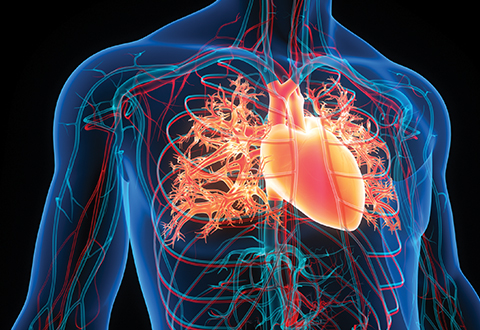
Chronic thromboembolic pulmonary hypertension (CTEPH) is a rare but severe form of pulmonary hypertension caused by unresolved blood clots in the pulmonary arteries. These clots obstruct blood flow, leading to increased pressure in the lungs and strain on the right side of the heart. Unlike other types of pulmonary hypertension, CTEPH is potentially curable with appropriate treatment.
Causes and Risk Factors
CTEPH develops as a complication of pulmonary embolism (PE) when blood clots fail to dissolve and become organized, resulting in chronic vascular obstruction. Common risk factors include:
- History of pulmonary embolism
- Clotting disorders, such as antiphospholipid syndrome
- Splenectomy
- Chronic inflammatory diseases, such as osteomyelitis
- Indwelling central venous catheters
It is essential to identify these risk factors early to facilitate timely diagnosis and management.
Symptoms of CTEPH
The symptoms of CTEPH often overlap with other forms of pulmonary hypertension, making diagnosis challenging. Common symptoms include:
- Persistent shortness of breath, especially during physical activity
- Fatigue and weakness
- Chest pain or discomfort
- Dizziness or fainting (syncope)
- Swelling in the legs and ankles (edema)
These symptoms tend to progress gradually, underscoring the importance of early detection.
Diagnostic Approaches
Diagnosing CTEPH involves a combination of clinical evaluation, imaging studies, and hemodynamic assessments. Key diagnostic methods include:
1. Ventilation/Perfusion (V/Q) Scan
A V/Q scan is the gold standard for detecting mismatched areas of ventilation and perfusion, characteristic of CTEPH.
2. CT Pulmonary Angiography (CTPA)
CTPA provides detailed imaging of the pulmonary vasculature to identify chronic thromboembolic lesions.
3. Right Heart Catheterization
This procedure measures pulmonary arterial pressure and confirms the diagnosis of pulmonary hypertension.
4. Pulmonary Angiography
This invasive imaging technique helps visualize vascular obstructions and assess their operability.
5. Echocardiography
Echocardiography evaluates right heart function and estimates pulmonary artery pressure, serving as a non-invasive screening tool.
Treatment Options
Effective treatment of CTEPH can significantly improve symptoms and prognosis. Available treatments include surgical, pharmacological, and interventional options.
1. Pulmonary Thromboendarterectomy (PTE)
PTE is the definitive treatment for CTEPH. This complex surgical procedure involves removing organized clots and fibrotic tissue from the pulmonary arteries. PTE offers a potential cure for eligible patients, with significant improvements in pulmonary hemodynamics and quality of life.
2. Balloon Pulmonary Angioplasty (BPA)
For patients ineligible for PTE or with residual pulmonary hypertension post-surgery, BPA is a minimally invasive procedure that dilates narrowed pulmonary arteries to improve blood flow.
3. Medical Therapy
Pharmacological treatment is used in patients with inoperable CTEPH or persistent pulmonary hypertension after PTE. Commonly used drugs include:
- Riociguat: A soluble guanylate cyclase stimulator that improves exercise capacity and pulmonary hemodynamics.
- Endothelin receptor antagonists (ERAs) and phosphodiesterase-5 inhibitors (PDE-5 inhibitors) for symptom management in select cases.
Long-Term Management and Follow-Up
Lifestyle Modifications
Patients with CTEPH benefit from:
- Regular exercise tailored to individual capacity
- A heart-healthy diet to manage comorbid conditions
- Smoking cessation to improve overall cardiovascular health
Regular Monitoring
Ongoing follow-up is crucial to assess treatment efficacy and detect potential complications. This includes periodic imaging, hemodynamic studies, and functional assessments.
Psychological Support
Living with a chronic condition can impact mental health. Access to counseling and support groups is invaluable for improving emotional well-being.
Prognosis
With advancements in diagnostic techniques and treatment modalities, the prognosis for CTEPH has significantly improved. Early detection and timely intervention remain key to achieving optimal outcomes.