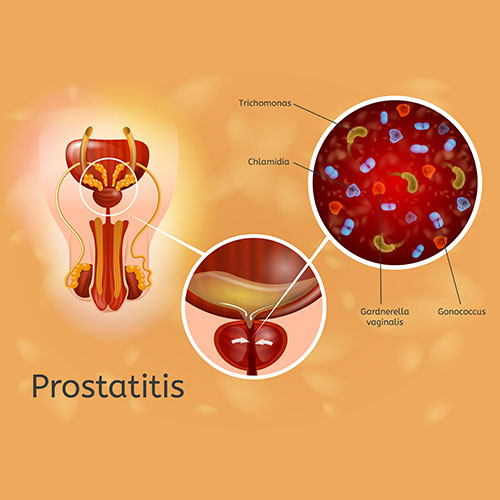
Chronic Staphylococcus epidermidis prostatitis is a persistent inflammation of the prostate gland caused by the bacterium Staphylococcus epidermidis. While commonly associated with skin flora, S. epidermidis can invade the prostate and cause significant discomfort and long-term complications. This article explores the causes, symptoms, diagnostic approaches, and treatment options for this condition, providing valuable insights for both patients and healthcare professionals.
Causes of Chronic Staphylococcus Epidermidis Prostatitis
Understanding Staphylococcus Epidermidis
Staphylococcus epidermidis is a coagulase-negative staphylococcus (CoNS) that resides harmlessly on the skin and mucous membranes. However, under specific circumstances, it can act as an opportunistic pathogen. Risk factors for infection include:
- Urinary Catheterization: Prolonged use of catheters increases susceptibility.
- Prostate Biopsies: Procedures involving the prostate may introduce S. epidermidis.
- Compromised Immunity: Conditions such as diabetes or immunosuppressive therapy.
- Biofilm Formation: S. epidermidis excels at forming biofilms, making infections challenging to eradicate.
Symptoms of Chronic Prostatitis
The clinical presentation of chronic S. epidermidis prostatitis can be subtle and prolonged. Common symptoms include:
- Pelvic Pain: Persistent discomfort in the perineal region.
- Urinary Issues: Increased frequency, urgency, dysuria, or weak stream.
- Sexual Dysfunction: Pain during ejaculation and reduced libido.
- General Malaise: Fatigue and low-grade fever may also occur.
These symptoms often overlap with other types of chronic prostatitis, necessitating accurate diagnosis.
Diagnosis of Chronic Staphylococcus Epidermidis Prostatitis
Clinical Evaluation
Diagnosis begins with a detailed patient history and physical examination, including a digital rectal exam (DRE) to assess prostate tenderness or enlargement.
Laboratory Tests
- Urinalysis and Culture: Midstream urine samples or post-prostatic massage urine can identify S. epidermidis.
- Prostate-Specific Antigen (PSA): Elevated PSA levels may indicate inflammation or infection.
Advanced Techniques
- Microbiological Cultures: Isolating S. epidermidis from prostatic secretions confirms the diagnosis.
- PCR Testing: Detects bacterial DNA with high sensitivity.
- Imaging: Ultrasound or MRI may help identify structural abnormalities or abscesses.
Treatment Options
Antibiotic Therapy
Targeted antibiotic treatment is the cornerstone of management. Commonly prescribed antibiotics include:
- Fluoroquinolones: Ciprofloxacin or levofloxacin.
- Trimethoprim-Sulfamethoxazole (TMP-SMX): Effective against S. epidermidis.
- Doxycycline: Useful in resistant cases.
Long-term antibiotic courses may be required due to the bacterium’s biofilm-forming capability.
Adjunctive Therapies
- Alpha-Blockers: Relieve urinary symptoms by relaxing prostate smooth muscles.
- Anti-Inflammatory Medications: NSAIDs reduce pain and inflammation.
- Pelvic Floor Physiotherapy: Alleviates chronic pelvic pain.
Surgical Interventions
For refractory cases or complications such as abscess formation, transurethral resection of the prostate (TURP) or abscess drainage may be necessary.
Preventive Measures
Minimizing Risk Factors
- Sterile Procedures: Ensuring sterile techniques during catheterization and biopsies.
- Hygiene Practices: Maintaining cleanliness to prevent bacterial spread.
- Regular Health Checkups: Early detection of urinary or prostate abnormalities.
Lifestyle Modifications
- Hydration: Adequate water intake supports urinary health.
- Balanced Diet: Anti-inflammatory foods, including fruits and vegetables, may help.
- Physical Activity: Regular exercise improves overall prostate health.
Prognosis and Long-Term Management
With timely and appropriate treatment, most patients experience symptom relief and reduced complications. However, recurrent infections remain a concern. Regular follow-ups and adherence to prescribed therapies are essential for long-term management.