Overview of Chronic Pulmonary Histoplasmosis
Chronic pulmonary histoplasmosis is a progressive fungal infection caused by Histoplasma capsulatum. This condition predominantly affects individuals with pre-existing pulmonary diseases, such as chronic obstructive pulmonary disease (COPD). The disease arises from inhaling fungal spores found in contaminated soil, particularly in regions with high concentrations of bird or bat droppings.
Etiology and Pathogenesis
Histoplasma capsulatum is a dimorphic fungus, existing as a mold in the environment and transforming into a yeast form at body temperature. The spores, when inhaled, travel to the alveoli, where they are engulfed by macrophages. The fungus can survive within macrophages, enabling dissemination to other parts of the lungs or even beyond, in severe cases. Chronic pulmonary histoplasmosis occurs when the fungal infection leads to sustained inflammation and tissue damage over time.
High-Risk Factors
- Individuals with structural lung diseases (e.g., COPD, emphysema)
- People living in endemic areas, particularly the Ohio and Mississippi River valleys
- Immunocompromised patients (e.g., due to HIV/AIDS or prolonged corticosteroid use)
Clinical Presentation
Symptoms
Patients with chronic pulmonary histoplasmosis may present with symptoms resembling tuberculosis. Common symptoms include:
- Persistent cough (often with sputum production or hemoptysis)
- Fever and chills
- Night sweats
- Fatigue and weight loss
- Chest pain
- Shortness of breath
Complications
If left untreated, chronic pulmonary histoplasmosis can lead to:
- Progressive lung fibrosis
- Bronchiectasis
- Respiratory failure
- Dissemination to extrapulmonary sites (rare)
Diagnosis
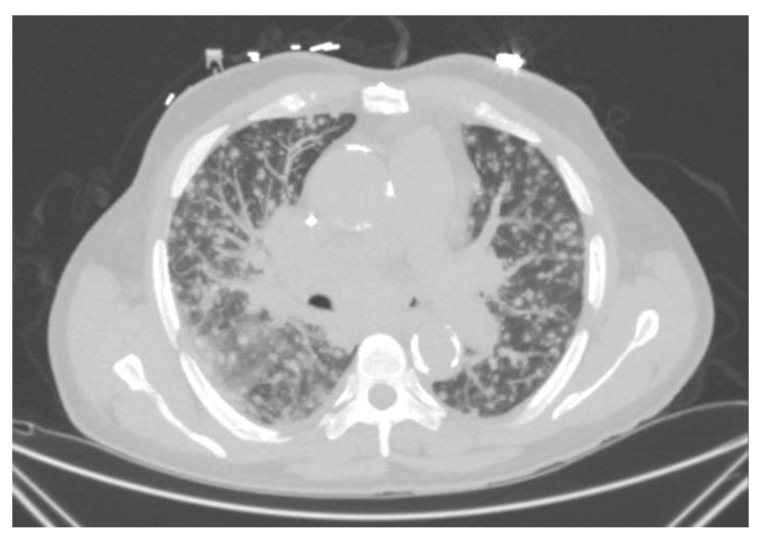
The diagnosis involves a combination of clinical, radiological, and laboratory evaluations.
Diagnostic Tests
- Chest Imaging
- Chest X-ray or CT scan typically reveals upper-lobe infiltrates, cavitation, or nodular lesions.
- Microbiological Testing
- Fungal Culture: Considered the gold standard, although it may take weeks to yield results.
- Histopathology: Identification of yeast forms within tissue samples.
- Serological and Antigen Testing
- Complement Fixation Test: Detects antibodies against Histoplasma antigens.
- Antigen Detection: Useful for detecting disseminated infections.
- Molecular Testing
- Polymerase chain reaction (PCR) assays for rapid detection of fungal DNA.
Differential Diagnosis
Chronic pulmonary histoplasmosis shares overlapping features with:
- Tuberculosis
- Non-tuberculous mycobacterial infections
- Lung cancer
- Sarcoidosis
Treatment
Antifungal Therapy
- Itraconazole: The first-line treatment, typically administered for 12-24 months.
- Amphotericin B: Reserved for severe or refractory cases, often as an induction therapy.
Adjunctive Therapies
- Corticosteroids: Occasionally used to manage severe inflammatory responses.
- Oxygen Therapy: For patients with significant hypoxemia.
Monitoring
Regular follow-up is essential to assess treatment efficacy, monitor for recurrence, and manage complications. Serial imaging and antigen testing are commonly employed.
Prevention
Environmental Precautions
- Avoid exposure to areas with high concentrations of bird or bat droppings.
- Use protective equipment, such as masks, when engaging in activities like construction or excavation in endemic regions.
Public Health Strategies
- Educate high-risk populations about the risks of exposure.
- Promote early detection and treatment in endemic areas.
Prognosis
With timely diagnosis and appropriate antifungal therapy, the prognosis for chronic pulmonary histoplasmosis is favorable for most patients. However, untreated or misdiagnosed cases may lead to severe complications and increased mortality.