Chronic myeloid leukemia (CML) is a rare but significant hematologic malignancy characterized by the uncontrolled growth of myeloid cells in the bone marrow. Among its distinct phases, the chronic phase (CP-CML) is the earliest and most manageable stage. In this article, we delve into the intricacies of CP-CML, exploring its symptoms, pathophysiology, diagnostic methods, treatment approaches, and prognostic considerations.
Understanding the Chronic Phase of CML
CML progresses through three distinct phases: chronic, accelerated, and blast phases. The chronic phase, which accounts for approximately 85% of initial diagnoses, is marked by a slower progression of the disease and relatively mild symptoms compared to later stages.
Pathophysiology of CP-CML
At the core of CML lies the Philadelphia chromosome, a genetic abnormality resulting from a translocation between chromosomes 9 and 22 (t[9;22]). This translocation generates the BCR-ABL1 fusion gene, which encodes a constitutively active tyrosine kinase that drives uncontrolled cell proliferation. In the chronic phase, the bone marrow remains capable of producing mature blood cells, albeit alongside the overproduction of myeloid cells.
Clinical Presentation and Symptoms
Many patients with CP-CML are asymptomatic and are diagnosed incidentally during routine blood tests. When symptoms are present, they may include:
- Fatigue
- Unexplained weight loss
- Night sweats
- Low-grade fever
- Splenomegaly, leading to abdominal discomfort
- Easy bruising or bleeding
Diagnostic Approach to Chronic phase chronic myeloid leukemia
Timely diagnosis of CP-CML is critical for optimal management. The diagnostic process typically involves:
Complete Blood Count (CBC)
A CBC often reveals leukocytosis with a marked increase in neutrophils and immature myeloid cells, basophilia, and sometimes thrombocytosis.
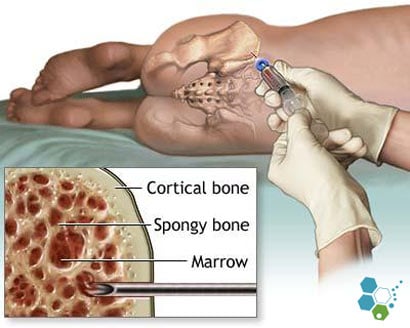
Bone Marrow Examination
Bone marrow aspirate and biopsy confirm hypercellularity with increased myeloid precursors. Morphological analysis helps assess disease phase.
Cytogenetic and Molecular Testing
- Karyotyping: Detects the Philadelphia chromosome in metaphase cells.
- Fluorescence In Situ Hybridization (FISH): Identifies BCR-ABL1 fusion in interphase cells.
- Quantitative Polymerase Chain Reaction (qPCR): Measures BCR-ABL1 transcript levels, providing a baseline for monitoring treatment response.
Treatment Strategies for CP-CML
The introduction of tyrosine kinase inhibitors (TKIs) has revolutionized the treatment landscape for CP-CML, transforming it into a manageable chronic condition for most patients.
First-Line Therapy: TKIs
TKIs target the BCR-ABL1 protein, inhibiting its activity and curbing disease progression. Commonly used TKIs include:
- Imatinib: The first TKI approved for CP-CML.
- Dasatinib and Nilotinib: Second-generation TKIs with higher potency and activity against imatinib-resistant mutations.
- Bosutinib and Ponatinib: Third-generation TKIs reserved for resistant or intolerant cases.
Monitoring Treatment Response
Regular monitoring is essential to evaluate therapeutic efficacy and adjust treatment as needed. Response milestones include:
- Hematologic Response: Normalization of blood counts within 3 months.
- Cytogenetic Response: Reduction or absence of Philadelphia chromosome-positive cells.
- Molecular Response: Decrease in BCR-ABL1 transcript levels.
Allogeneic Hematopoietic Stem Cell Transplant (HSCT)
Although rarely required in the chronic phase, HSCT remains an option for patients with TKI resistance or intolerance.
Prognosis and Long-Term Management
The prognosis for CP-CML has improved dramatically with TKI therapy. Most patients achieve long-term remission with minimal side effects. Adherence to treatment and regular monitoring are critical for sustained success.
Common Challenges
- TKI resistance due to BCR-ABL1 mutations.
- Adverse effects such as fatigue, edema, and gastrointestinal symptoms.
- Financial burden associated with prolonged TKI use.
Emerging Therapies
Ongoing research aims to develop novel therapies to overcome resistance, reduce toxicity, and potentially achieve treatment-free remission (TFR) in eligible patients.