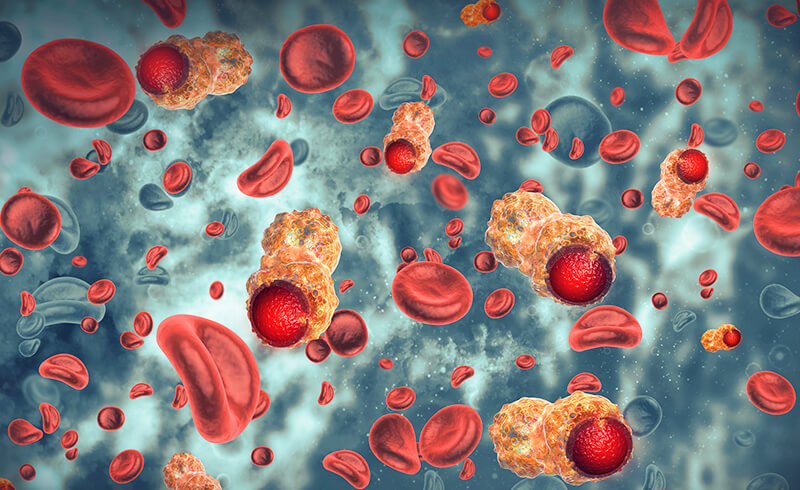
Chronic myelomonocytic leukemia (CMML) is a type of cancer that affects blood-forming cells of the bone marrow and the monocytes, which are a type of white blood cell. Unlike acute leukemias, CMML develops slowly and progresses at a more gradual rate, which makes its diagnosis and management particularly challenging. This article delves into the essential aspects of CMML, including its symptoms, causes, diagnostic methods, treatment options, and long-term management strategies.
What is Chronic Myelomonocytic Leukemia (CMML)?
Chronic myelomonocytic leukemia (CMML) is classified as a type of leukemia, a cancer that originates in blood-forming tissues. It is a rare and unique form of leukemia that has features similar to both chronic myelogenous leukemia (CML) and acute myelomonocytic leukemia (AML), making it more difficult to diagnose and categorize. CMML primarily affects the bone marrow, where it disrupts the normal production of blood cells, leading to an overproduction of monocytes and other immature white blood cells.
Key Characteristics of CMML:
- Slow progression: CMML usually develops over time, with the symptoms often appearing gradually.
- Monocyte overproduction: The disease is characterized by an excessive number of monocytes in the blood, which can interfere with normal blood cell production.
- Chronic nature: Unlike acute leukemia, which progresses quickly, CMML often remains stable for long periods, though it may transform into a more aggressive form over time.
Symptoms of Chronic Myelomonocytic Leukemia
The symptoms of CMML can vary significantly between individuals, and early-stage cases may not show obvious signs. However, as the disease progresses, the following symptoms are commonly observed:
Common Symptoms:
- Fatigue and weakness: Due to reduced red blood cell count, patients may experience general fatigue and weakness.
- Frequent infections: The overproduction of white blood cells may lead to a compromised immune system, making patients more susceptible to infections.
- Paleness: Anemia caused by low red blood cell counts may result in pale skin.
- Fever and night sweats: These symptoms are often associated with infections or the progression of the disease itself.
- Enlarged spleen (splenomegaly): The spleen may become enlarged due to the accumulation of abnormal blood cells.
- Enlarged liver (hepatomegaly): Similarly, the liver can become swollen, contributing to discomfort or pain in the abdomen.
Causes and Risk Factors of CMML
The precise cause of chronic myelomonocytic leukemia remains unknown, but certain factors can increase the risk of developing this type of leukemia:
Possible Causes:
- Genetic mutations: Research has shown that mutations in specific genes, such as the TET2, ASXL1, and SRSF2 genes, may play a role in the development of CMML.
- Chronic exposure to toxins: Long-term exposure to chemicals like benzene and certain pesticides has been linked to an increased risk of developing leukemia.
- Previous chemotherapy or radiation: Patients who have undergone certain cancer treatments, such as chemotherapy or radiation therapy, may be at a higher risk of developing CMML.
- Age and gender: CMML is more commonly diagnosed in older adults, and it tends to affect men more frequently than women.
Diagnosing Chronic Myelomonocytic Leukemia
The diagnosis of CMML involves a series of tests to evaluate blood counts, bone marrow samples, and genetic markers. These methods help differentiate CMML from other forms of leukemia and blood disorders.
Diagnostic Methods:
- Blood tests: A complete blood count (CBC) is typically the first test used. It measures the number of red blood cells, white blood cells, and platelets, helping to identify abnormal counts.
- Bone marrow biopsy: A sample of bone marrow is taken to examine the number of monocytes and other blood cells present. This test is crucial in confirming a diagnosis of CMML.
- Cytogenetic testing: This test looks for genetic mutations or abnormalities in the chromosomes of leukemia cells.
- Flow cytometry: This technique is used to examine the surface markers on white blood cells to help classify the leukemia type.
Treatment Options for Chronic Myelomonocytic Leukemia
There is no standard treatment for CMML, and the management plan depends on the patient’s age, general health, and the specific characteristics of the disease. Treatment approaches aim to control symptoms, prevent complications, and slow the progression of the disease.
Treatment Modalities:
- Chemotherapy: Chemotherapy drugs may be used to target and kill the abnormal blood cells. However, chemotherapy is often less effective in CMML compared to other types of leukemia.
- Targeted therapy: Targeted drugs that focus on specific genetic mutations within the leukemia cells can be used. These therapies are more precise and tend to have fewer side effects than traditional chemotherapy.
- Stem cell transplant: In some cases, a stem cell or bone marrow transplant may be recommended, especially for patients who have relapsed or have aggressive disease.
- Immunotherapy: Immunotherapies aim to boost the body’s immune response against leukemia cells and are being explored as potential treatment options for CMML.
- Supportive care: Medications to manage pain, prevent infections, and address anemia or bleeding tendencies may also be used to improve the quality of life.
Prognosis and Long-Term Management
The prognosis for patients with chronic myelomonocytic leukemia can vary widely. Many individuals live with the disease for many years, particularly if it remains stable. However, CMML can transform into acute myeloid leukemia (AML), which is more aggressive and harder to treat.
Key Prognostic Factors:
- Age and overall health: Younger patients in good general health often have a better prognosis.
- Genetic mutations: Certain genetic mutations are associated with more favorable or unfavorable outcomes.
- Response to treatment: How well the disease responds to initial treatments can influence long-term survival.
Long-term management typically involves regular monitoring of blood counts, bone marrow function, and periodic genetic testing to assess disease progression. Patients may require adjustments to their treatment plan depending on the course of the disease.