Chronic lymphocytic leukemia (CLL) with 17p deletion represents a unique and high-risk subset of this hematologic malignancy. The 17p deletion encompasses the TP53 gene, critical for cellular DNA repair and apoptosis. Patients with this genetic aberration often exhibit resistance to standard therapies, leading to poorer outcomes. This article provides a detailed analysis of CLL with 17p deletion, from pathophysiology to emerging treatments.

Understanding 17p Deletion in CLL
Pathophysiology
The 17p deletion involves the loss of a portion of chromosome 17, specifically the region harboring the TP53 gene. The TP53 gene encodes the p53 protein, often referred to as the “guardian of the genome.” This protein is essential for regulating cell cycle arrest, DNA repair, and apoptosis in response to genomic damage. When this gene is lost or mutated, malignant cells proliferate unchecked, contributing to CLL progression.
Epidemiology
- Incidence: Approximately 5-10% of newly diagnosed CLL cases exhibit 17p deletion, increasing to 30-50% in refractory or relapsed disease.
- Risk Factors: Age, prior therapy, and disease stage may influence the emergence of 17p deletion.
Clinical Presentation
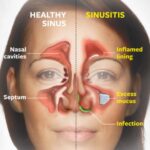
Patients with CLL and 17p deletion often present with:
- Aggressive Disease Course: Rapid lymphocyte proliferation and shorter time to treatment.
- Refractoriness to Standard Therapy: Poor response to traditional chemotherapies, such as fludarabine-based regimens.
- Symptoms: Fatigue, lymphadenopathy, splenomegaly, recurrent infections, and night sweats are common.
Diagnostic Approach
Genetic Testing
Accurate diagnosis of 17p deletion in CLL requires cytogenetic and molecular studies:
- Fluorescence In Situ Hybridization (FISH): Gold standard for detecting 17p deletions.
- Next-Generation Sequencing (NGS): Detects concurrent TP53 mutations, often coexisting with 17p deletion.
Hematological Evaluation
Routine blood tests often reveal:
- Elevated lymphocyte counts (>5,000/µL)
- Anemia and thrombocytopenia in advanced stages
Prognosis of CLL with 17p Deletion
17p deletion is associated with:
- Shorter Progression-Free Survival (PFS): Median PFS of less than two years with traditional treatments.
- Reduced Overall Survival (OS): Median OS of 3-5 years without advanced therapies.
Treatment Strategies for CLL with 17p Deletion
Targeted Therapies
The advent of targeted treatments has significantly improved outcomes:
- Bruton Tyrosine Kinase (BTK) Inhibitors:
- Examples: Ibrutinib, Acalabrutinib
- Mechanism: Block BTK signaling, preventing CLL cell survival.
- BCL-2 Inhibitors:
- Example: Venetoclax
- Mechanism: Induces apoptosis by inhibiting BCL-2, a protein that prevents cell death.
- PI3K Inhibitors:
- Examples: Idelalisib, Duvelisib
- Mechanism: Target the PI3K pathway, critical for CLL cell proliferation.
Monoclonal Antibodies
- Examples: Rituximab, Obinutuzumab
- Often combined with targeted agents for enhanced efficacy.
Chimeric Antigen Receptor (CAR) T-Cell Therapy
Emerging as a potential option for refractory cases, CAR T-cell therapy uses genetically modified T cells to target and eliminate CLL cells.
Allogeneic Stem Cell Transplantation
Reserved for younger, fit patients with refractory disease, offering the potential for long-term remission.
Monitoring and Follow-Up
Minimal Residual Disease (MRD) Assessment
- Detects low levels of CLL cells post-treatment using flow cytometry or molecular techniques.
- MRD negativity correlates with improved survival.
Regular Clinical Assessments
- Blood counts, imaging studies, and physical exams to monitor disease progression.
Future Directions in Research
Novel BTK Inhibitors
- Next-generation BTK inhibitors aim to overcome resistance and improve safety profiles.
Combination Therapies
- Synergistic combinations of targeted agents to enhance efficacy and reduce resistance.
Biomarker Development
- Identification of biomarkers predicting therapy response and disease progression.